Background: Tumor lysis syndrome (TLS) is a feared complication particularly among patients of diffuse large B cell lymphoma (DLBCL) with bulky lymphadenopathy. We conducted a national wide retrospective analysis to determine the impact of TLS on hospitalization among patients admitted for treatment of DLBCL.
Methods: The data for this study was obtained from the National Inpatient Sample Database. Using the relevant International Classification of Diseases (1CD) 10 codes, hospitalizations with the primary diagnosis of DLBCL from 2015-19 were subclassified into cases with and without TLS. Univariate analysis was conducted using the chi-square and T-test to compare categorical and continuous variables, respectively between the two groups. Thereafter, propensity score matching (PSM) was performed to match the two groups for patient demographics, and comorbidities. Cochran-Mantel-Haenzel test was used for determining the odds ratio between the endpoints of interest. A p value of <0.05 was considered significant. The primary endpoint was the difference in all-cause mortality between the two matched cohorts. Other secondary endpoints included important hospitalization complications like acute kidney injury (AKI), cardiac arrhythmias (CA), renal failure requiring hemodialysis (HD), and respiratory failure requiring mechanical ventilation (MV). We also performed cost analysis to determine the difference in length of stay (LOS) and adjusted cost of stay between the two groups.
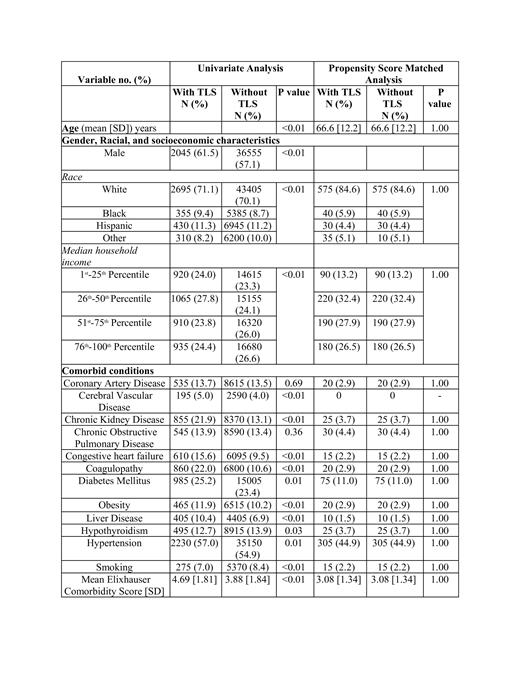
Results: A total of 67910 weighted hospitalizations with a primary diagnosis of DLBCL were recorded from 2015-2019. Among these 3910 (5.8) hospitalizations had TLS.Cases with TLS were more likely to be male (61.5% vs57.1; p<0.01) and black (9.4% vs 8.7%, p<0.01). There was a higher proportion of patients with comorbid conditions in the TLS cohort compared to the no TLS cohort, notably history of coagulopathy (22% vs 10.6%), chronic kidney disease (21.9% vs 13.1%), congestive heart failure (15.6% vs 9.5%), diabetes (25.2% vs 23.4%), liver disease (10.4% vs 6.9%), and hypertension (57.0% vs 54.9%) (all p<0.01) (Table 1). After PSM adjusted for these baseline differences, 680 cases of TLS were matched with 680 cases without TLS. Hospitalizations with TLS had higher odds of all-cause mortality (Odds Ratio [OR] = 2.89, 95% confidence interval [CI]: 1.87-4.46; p<0.01). Patients with TLS also had higher odds of AKI (OR = 5.77, 95% CI: 4.53-7.35; p<0.01), HD (OR = 3.63, 95% CI: 1.79-7.40; p <0.01), and MV (OR = 3.79, 95% CI: 2.28-6.30; p<0.01). Though there was a trend towards higher odds of CA, the difference was not statistically significant. Patients with TLS also had a higher mean LOS (12.2 vs 10.8 days, p<0.01), and mean adjusted cost of hospitalization ($53933 vs $36958, p<0.01) (Table 2).
Conclusions: Patients with DLBCL that develop TLS are at a higher risk of all-cause mortality and morbidity. Preventive strategies like generous hydration and early detection of TLS are pivotal to improve outcomes.
Disclosures
Jaglal:Agios: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees; SOBI: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal